download the brief
Key Findings



The opioid crisis besetting every region of the United States directly affects more than just those who use substances. For a pregnant woman, a consequence of substance use can be neonatal abstinence syndrome (NAS)—withdrawal symptoms experienced by the newborn (see Box 1).
NAS is on the rise in New Hampshire, but prenatal care for the mother can reduce or eliminate the risk. Newborns who are treated recover, yet mothers using opioids are often using other substances and confronting behavioral health issues which complicate recovery.
This brief analyzes inpatient hospital discharge data (2012–2015) to assess the prevalence of NAS in New Hampshire; describes one hospital’s successful program for treating pregnant women and newborns; discusses how comprehensive and coordinated care and home visiting services provided through community based organizations can support new mothers and families; and discusses how a recent change to New Hampshire law intended to support child protection may be having unintended consequences.
Opioid Drug Use and NAS in New Hampshire
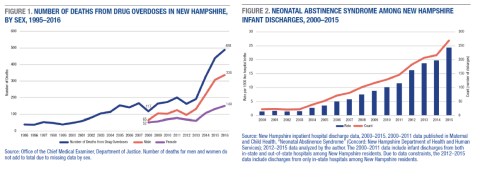
Drug overdose deaths are on the rise in New Hampshire. In 2016, the state medical examiner reported 488 deaths from drug overdoses, up from 192 just four years earlier (Figure 1).1 Overdose deaths among women nearly tripled between 2008 and 2016, from 52 to 149. However, because the incidence of drug overdose death among men grew at a faster pace, women represented a smaller proportion of overdose deaths in 2016 (31 percent) than in 2008 (44 percent).2
Opioid-related emergency department visits can be used to estimate opioid use. In 2016, there were 2,632 female and 3,452 male visits,3 and they were most prevalent among 20–29-year-olds and 30–39-year-olds, the typical child-bearing years for women.
An increase in maternal drug use accounts for a rise in the number of newborns diagnosed with NAS. The rate of NAS in the United States rose from 1.2 per every 1,000 hospital births in 2000 to 5.8 per 1,000 in 2012,4 leading many to call perinatal opioid use a national public health crisis.5 In New Hampshire, NAS has increased fivefold since the early 2000s (Figure 2). In 2015, 269 infants were diagnosed with NAS, compared to 52 in 2005.6 This number may be an underestimate, because hospitals may report NAS differently depending on provider documentation and coding of diagnosis, and also issues of data quality.7 Figure 2 also shows that the rate of NAS births per 1,000 live hospital births reached 24.4 per 1,000 in 2015. In other words, at least 2.4 percent of live New Hampshire births in 2015 were diagnosed with NAS.
In 2015, New Hampshire newborns diagnosed with NAS remained in the hospital on average twelve days, owing to some needing monitoring and care while they were weaned off opiates, compared to three days for newborns not born exposed. However, not all newborns with NAS needed intensive services, and 41 percent were able to leave the hospital within five days.
Early Successes in Addressing NAS
Hospitals are responding to the increased prevalence of NAS in different ways. Some offer prenatal comprehensive and coordinated care, including medication-assisted treatment, while others have instituted postnatal infant cuddling programs, since skin-to-skin contact is important for infants during withdrawal and recovery. Since 2015 (the time of data collection), several New Hampshire hospitals have instituted protocols for NAS intervention that have shortened the length of stay for newborns with NAS.
The Dartmouth-Hitchcock Medical Center (DHMC) launched one of the first programs in New Hampshire, the Moms in Recovery program, in 2013 to address the need for access to treatment among pregnant women who were using opiates. Moms in Recovery uses an integrated model to provide outpatient medication-assisted treatment, maternity care, maternal behavioral health care, referrals to community services, and case management. Participants attend group treatment sessions focused on addiction treatment and education and receive individual visits for medication, individual therapy, case management, and prenatal care.
DHMC reports that its program has been successful in achieving positive maternal and neonatal outcomes, and in some cases the birth outcomes are comparable to the overall population of births. For example, fewer than 25 percent of infants born to DHMC Moms in Recovery participants require treatment for NAS; the length of stay for neonates requiring treatment has declined by three days since 2013, and about 80 percent of program participants initiate breastfeeding.8
In 2015, 7.8 percent of newborns to New Hampshire residents at DHMC were diagnosed with NAS, a higher proportion than the statewide average of 2.4 percent,9 but NAS births at DHMC had a shorter length of stay compared with other New Hampshire hospitals—8.3 versus 13.3 days.10 Although not conclusive, these data suggest that DHMC’s programs are reducing the length of the hospital stay for newborns with NAS.
NAS births are more costly on average than other births, likely owing to longer hospital stays.11 In 2015, the total discharge amount for all births coded with an NAS diagnosis in New Hampshire averaged $33,700, compared to $7,800 for those not diagnosed with NAS.12 Medicaid covered 78 percent of NAS births in 2013.13
Increase and Target Services to Address NAS Statewide
During pregnancy, women who are drug dependent often voice motivation to stop using drugs and to seek treatment.14 Thus, pregnancy provides an opportune time for health care providers and hospitals to initiate services and provide referrals, and there are a variety of options.
Community-based nonprofit service organizations15 are at the front line of the opioid crisis, providing services on a voluntary basis to families in need. Services support and promote family health and well-being through education and prevention, often in collaboration with other social service agencies and local public and private organizations. Programs offered typically include health education, safety, and injury prevention; assistance with enrollment in health insurance, nutrition programs, or child care payment assistance programs; family mentoring, parenting, and child development education; domestic violence prevention and interventions services; and home visiting.
Home visiting has been shown to improve maternal and infant health, increase children’s school readiness and safety, and improve family self-sufficiency.21 Two state-wide programs operate on a contract basis through community-based nonprofit service organizations: the Maternal Infant and Early Childhood Home Visiting Program (MIECHV), which is under the Maternal and Child Health Section of the New Hampshire Department of Health and Human Services; and Comprehensive Family Support Services (CFSS), under the Department of Children, Youth, and Families. A small portion of the CFSS home visiting program is paid for by Medicaid.
MIECHV uses the Healthy Families America model, a research-based voluntary home visiting program that targets families most at risk of child maltreatment and adverse childhood experiences. Many of the families receiving MIECHV services struggle with substances: an evaluation of New Hampshire’s Healthy Families America found that 37 percent of caregivers served by the program were assessed as “known or suspected of substance misuse.”22 Families voluntarily enroll in services prenatally or within two weeks after a child’s birth, and services span up to the child’s third birthday with the goal of promoting healthy child development and preventing child abuse and neglect. In 2016, MIECHV served 325 families at 11 sites, for a total of 4,639 home visits.23 It is important to note that in October 2017 Congress let the MIECHV program expire.
Families with a child under 21 are eligible to participate in CFSS voluntary services, which include home visiting and other programs offered by community-based nonprofit service organizations. Families voluntarily request services, and a service plan is initiated. In 2015, 1,048 New Hampshire families participated in CFSS, with 3,430 family members served, including 1,926 children.24
For those who are eligible, CFSS voluntary home visiting services can be charged to the Medicaid home visiting program, Home Visiting New Hampshire, which has strict eligibility guidelines. All mothers with infants diagnosed with NAS are eligible, as long as they are Medicaid recipients, first-time mothers, and under the age of 21 enrolling in the program no more than two weeks after the child’s birth. Services can be provided up to the child’s first birthday. Many families are likely not aware of these services because hospitals typically give referrals for outside services at discharge, and providers may shy away from referrals for services that are associated with the Department of Children, Youth, and Families. Moreover, Medicaid’s strict home-visiting guidelines translate into few families being eligible for and enrolling in the program. Loosening the age restriction, allowing home visits at the time of any birth, and lengthening the signup period would expand access to more families.
Working with hospitals, maternal health care providers, and pediatricians to encourage referrals to home visiting for newborns diagnosed with NAS and their families could be an important first step in ensuring continued child health. Offering pre- and postnatal home visits to all families could reduce stigma and go a long way toward helping all new parents in the first days home with a new baby.
Challenges to Addressing NAS Statewide
Pregnant women are reluctant to disclose their opioid use because of the stigma associated with using substances, especially while pregnant, and because of the fear that a provider will report their substance use to Child Protective Services, resulting in their child being taken away and their parental rights terminated.25 Yet mothers who do not disclose suffer in silence and do not get the care and services they need, and their newborns have longer, harder recoveries in the hospital.
In order to address NAS, legislators, advocates, and health care providers are calling for a shift away from punitive attitudes toward treatment in an effort to reduce shame and encourage compliance among pregnant women. A successful approach to this problem will be one that treats both the mother and the newborn with comprehensive and coordinated care, provides home visiting and other services to build confidence in parenting and to spot issues before they spiral into problems, and has a supportive peer and community network. Yet, New Hampshire also needs to ensure that children are protected from harm. Parental drug use endangers children’s health and safety in the short and long term. Children who face adverse childhood experiences such as parental addiction and drug use have an elevated risk of using drugs at age 14 and of continuing that use into adulthood.26
Unintended Consequences of Policy Change
In an effort to give the Department of Children, Youth, and Families discretion and a legal basis for intervention before harm occurs, in June 2016 New Hampshire amended its Child Protection Act to create “a rebuttable presumption that the child’s health has suffered or is very likely to suffer serious impairment” from a parent’s drug use and so shifts the responsibility to parents to provide evidence of their compliance with drug use treatment.27 A pregnant woman could use participation in medication-assisted treatment as evidence of compliance. The bill does not conclude that a parent is neglectful if abusing drugs, nor does it require departmental involvement or mandate removal of a child. The stated intent is to give the department discretion and to encourage treatment as a way to promote the unity of the family when possible.28
However, there is persuasive anecdotal evidence of a misunderstanding of the intent of the law by parents and within the health care, social service, and court systems. This confusion surrounds the interpretation of mandatory reporting of child neglect to the Department of Children, Youth, and Families. Unintended consequences may include a chilling effect on women seeking prenatal care, their willingness to disclose during pregnancy, and reporting by providers. Any of these consequences are detrimental to newborns if pregnant women do not get the treatment and care they need. More research is needed to determine how the law has been interpreted by parents and professionals and, in the wake of those findings, identify steps to clarify any misinterpretation.
Conclusions
In 2015, 2.4 percent of New Hampshire births were diagnosed with NAS, and that number is projected to rise, with implications for early intervention programs, early education programs, and primary schools. Children born drug-exposed are at increased risk for behavioral health problems, especially if their parents continue using. Pregnancy is a time to reach out to mothers, as they are more receptive to services and making a change. Reaching out when their children are young to initiate treatment, provide services, and shore up community supports within a coordinated care and case management framework can be in the best interest of the child’s health and safety.
Yet, mothers using opioids are often also using other substances, including alcohol, cigarettes, marijuana, and other illicit drugs, and are often confronting issues related to mental health, poverty, homelessness, and/or domestic violence—all of which complicate recovery. Policies and programs should not consider opioid addiction in isolation, but rather as one interconnected symptom within a larger context. Both alcohol and tobacco use during pregnancy have proven negative health consequences for children, and the adverse effects on children are magnified when combined with opiates. Getting mothers on a path to recovery is a formidable challenge facing our state, but one that ultimately will help children and promote family unity.
Data
All hospitals licensed by the New Hampshire Department of Health and Human Services (DHHS) are required by law to report patient-level discharge information to DHSS. Information collected includes, but is not limited to, hospital, patient demographic characteristics, admission type, admitting diagnosis, procedure codes, length of stay, primary payer, and total discharge cost received from the thirty-two reporting hospitals. The 2000–2011 data come from the DHHS Maternal and Child Health publication, “Neonatal Abstinence Syndrome,” and include infant discharges from both in-state and out-of-state hospitals among New Hampshire residents. Due to data constraints, the 2012–2015 data include discharges among only in-state hospitals among New Hampshire residents. For consistency in the trend line, we use the methodology employed by Maternal and Child Health (2015) and Patrick et al. (2015), which includes all infants under 1 coded with a NAS diagnosis in the discharge data. For comparisons across hospitals, we include newborns coded with a NAS diagnosis in the discharge data.
Box 1: What Is NAS?
Neonatal abstinence syndrome is a set of conditions occurring when a newborn experiences withdrawal symptoms after birth from drug exposure before birth. It is most often caused by opioids.16 Symptoms appear shortly after birth and include irritability, problems feeding, watery stools, overly toned muscles, tremors, seizures, and/or breathing problems.17 Data from prenatal care and treatment programs show that birth outcomes are better when pregnant women who are using drugs participate in prenatal care and undergo substance use treatment. Negative birth outcomes such as neonatal withdrawal, prematurity, fetal demise, and low birth weight are reduced when medication-assisted treatment, such as administration of methadone or buprenorphine, is prescribed during pregnancy.18 NAS can be treated or managed in the hospital after birth, and infants who are treated recover. The long-term effects of prenatal exposure are difficult to determine because of the challenge of isolating the independent effect of prenatal opiate exposure, prenatal co-exposure to other substances (tobacco, alcohol, other illicit drugs), and behavioral health and environmental factors (mental health, poverty, poor prenatal care).19 While the research is inconsistent as to the long-term consequences of NAS, studies consistently show that children diagnosed with fetal alcohol syndrome demonstrate delays in motor functions, poor coordination, delays in fine motor skills, and cognitive disability that persists into childhood.20
Endnotes
1. Office of the Chief Medical Examiner, Department of Justice. Data received from Kim Fallon, Chief Forensic Investigator, Office of the Chief Medical Examiner, NH.
2. Office of the Chief Medical Examiner, Department of Justice. Data received from Kimberly Fortier, New Hampshire Information and Analysis Center.
3. New Hampshire Division of Public Health Services, Automated Hospital Emergency Department Data (de-duplicated). Data received from Kimberly Fortier, New Hampshire Information and Analysis Center.
4. S.W. Patrick et al., “Increasing Incidence and Geographic Distribution of Neonatal Abstinence Syndrome: United States 2009 to 2012,” Journal of Perinatal 35 (2015): 650–55.
5. Maternal and Child Health, “Neonatal Abstinence Syndrome,” New Hampshire Department of Health and Human Services, Concord, NH, 2015; Julie Frew, Daisy Goodman, and Katrin Tchana, “Building a Life Worth Living: Treating Moms With Opioid Use Disorders,” presentation to the New Hampshire Association for Infant Mental Health, Concord, NH, 2017.
6. The 2000–2011 data include infant discharges from both in-state and out-of-state hospitals among New Hampshire residents. Due to data constraints, the 2012–2015 data include discharges among only in-state hospitals among New Hampshire residents.
7. There may be inconsistencies across New Hampshire hospitals in how they code NAS diagnoses on the discharge records depending on whether or not the newborn requires pharmacologic treatment. Infants whose mothers participated in medication-assisted treatment typically have less severe NAS symptoms and are less likely to require medication, thus some providers may not code these infants with an NAS diagnosis. Using the inpatient hospital discharge data, it is not possible at this time to distinguish whether opioid-using pregnant women participated in medication-assisted treatment.
8. Frew, Goodman, and Tchana, 2017. Email correspondence with Daisy Goodman revealed that 90 percent of mothers not in the program initiated breastfeeding, not a statistically significant difference from the 80 percent of program participants who initiated breastfeeding.
9. Author’s analysis of New Hampshire hospital inpatient discharge data. This percentage is similar to DHMC internal data provided by Daisy Goodman.
10. This difference is statistically significant at the p <.01 level. Current 2017 length-of-stay times are likely shorter than the 2015 average due to the protocols for NAS intervention that were put in place since 2015 in many New Hampshire hospitals.
11. A.V. Holmes et al., “Rooming-In to Treat Neonatal Abstinence Syndrome: Improved Family-Centered Care at Lower Cost,” Pediatrics 137, no. 6 (2016): e20152929.
12. Author’s analysis of New Hampshire hospital inpatient discharge data.
13. Author’s analysis of New Hampshire hospital inpatient discharge data.
14. Frew, Goodman, and Tchana, 2017.
15. Community-based nonprofit service organizations include but are not limited to family resource centers, child and family services, community action programs, and home visiting nurses associations. We use the term community-based nonprofit service organizations as an overarching term to capture all of these types of service providers.
16. NAS is associated with other substances besides opiates, including street drugs such as heroin and non-opioid prescription drugs such as antidepressants or benzodiazepines. But opiates such as codeine, hydrocodone, morphine, oxycodone, and tramadol are the main contributor; see Beth A. Logan, Mark S. Brown, and Marie J. Hayes, “Neonatal Abstinence Syndrome: Treatment and Pediatric Outcomes,” Clinical Obstetrics and Gynecology 56, no. 1 (2013): 186–192.
17. Maternal and Child Health, 2015.
In some cases, symptoms appear after one week.
18. Holmes et al., 2016.
19. D.S. Messinger et al., “The Maternal Lifestyle Study: Cognitive, Motor, and Behavioral Outcomes of Cocaine-Exposed and Opiate-Exposed Infants Through Three Years of Age,” Pediatrics 113, no. 6 (2004): 1677–85.
20. Barry M. Lester, Lynne Andreozzi, and Lindsey Appiah, “Substance Use During Pregnancy: Time for Policy to Catch Up With Research,” Harm Reduction Journal 1 (2004): 1–5.
21. Child and Family Research Partnership, “The Top 5 Benefits of Home Visiting Programs,” Lynden B. Johnson School of Public Affairs, University of Texas at Austin, 2015.
22. Reported by principal investigator Tobey Partch-Davies of the University of New Hampshire Institute on Disability.
23. Human Resources and Services Administration, MIECHV Home Visiting Program, New Hampshire, accessed 2017, https://mchb.hrsa.gov/sites/default/files/mchb/MaternalChildHealthInitia....
24. Presentation by Thom O’Connor, Division for Children, Youth and Families Family Resource Center Program, 2016.
25. Lester, Andreozzi, and Appiah, 2004.
26. Shanta R. Dube, Vincent J. Felitti, Maxia Dong, Daniel P. Chapman, Wayne H.Giles, and Robert F. Anda, “Childhood Abuse, Neglect, and Household Dysfunction and the Risk of Illicit Drug Use: The Adverse Childhood Experiences Study,” Pediatrics 111, no. 3 (March 2003): 564–72.
27. Senate Bill 515, relative to the child protection act, New Hampshire General Court, Concord, NH, 2016, http://www.gencourt.state.nh.us/bill_status/billText.aspx?sy=2016&id=906....
28. Senate Health and Human Services Committee, “SB 515-FN, relative to child neglect and other changes to the child protection act,” hearing of February 16, 2016.
Acknowledgements
The author thanks Michael Ettlinger, Curt Grimm, Michele Dillon, Eleanor Jaffee, Marybeth Mattingly, Jessica Carson, Amy Sterndale, Katie Fish, Laurel Lloyd, and Bianca Nicolosi at the Carsey School of Public Policy; Michele Merritt and Rebecca Woitkowski at New Futures; David Laflamme at New Hampshire Maternal and Child Health and the University of New Hampshire; Deborah Schachter and Tym Rourke at the New Hampshire Charitable Foundation; Daisy Goodman at Dartmouth Hitchcock Medical Center; Jonathan Stewart at John Snow, Inc.; and Patrick Watson for substantive comments and editorial contributions. The author also thanks the medical examiner’s office and the New Hampshire Information and Analysis Center for providing data, and over 40 individuals working on the front lines of the opioid epidemic who shared their expertise with the author.