Key Findings



As the incidence of COVID-19 accelerates and the pandemic spreads, attention has remained focused on urban America,1 where the bulk of the cases and deaths have occurred. But rural America is at considerable risk as well because the virus there is spreading rapidly.2
The risk of hospitalization or death to a community’s population from exposure to the coronavirus is influenced by social and demographic characteristics including age, pre-existing health conditions, inequality, poverty, food insecurity, race/Hispanic origin, and access to health care. However, two of these factors—age and pre-existing conditions—are known to have a substantial impact on the severity of and mortality associated with the coronavirus. Research documents that age-specific mortality rates from COVID-19 infection are consistently very low for younger age cohorts and much higher for the oldest cohorts. A strong association also exists between an individual having pre-existing health conditions and serious COVID-19 risks.3 Areas where pre-existing health conditions are widespread and the population is older face an increased likelihood of serious consequences from coronavirus infection. This fact puts many rural counties at greater risk because they have older populations with high rates of pre-existing health conditions.
This brief delineates the likely influence that the local age structure and the incidence of pre-existing health conditions have on the risks of those exposed to COVID-19 in rural and urban counties in the United States.4
Definition: “Risk” is defined here as the likelihood of hospitalization or death from COVID-19 infection. Those at high risk have a greater estimated likelihood of hospitalization or death as a result of exposure to COVID-19.
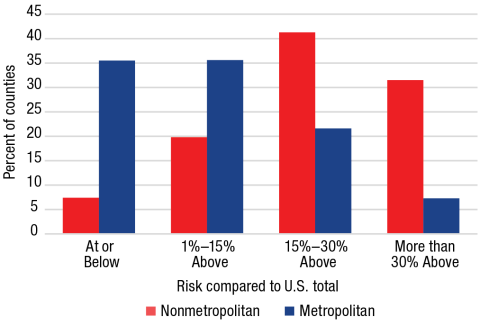
The risks associated with COVID-19 are greater among those with pre-existing health conditions who are infected. The Centers for Disease Control and Prevention estimates that, among those exposed to COVID-19, hospitalization was six times more likely and deaths were twelve times more likely among those with underlying conditions than among those without. Nonmetropolitan counties have a higher incidence of pre-existing health conditions than do metropolitan counties:5 nearly 33 percent of nonmetropolitan counties have populations with an incidence of pre-existing health conditions at least 30 percent above that in the United States as a whole compared to just 11 percent of metropolitan counties. In contrast, only 10 percent of nonmetropolitan counties have a lower incidence of pre-existing conditions than the United States overall compared to 35 percent of metropolitan counties. This puts nonmetropolitan America at greater risk if infections become widespread there.
A second major risk factor making the rural population more vulnerable to the virus is that it is considerably older than the urban population. More than 26 percent of the nonmetropolitan population is 60 or older compared to 21 percent of the metropolitan population. Among those infected, both mortality and the severity of the virus are significantly higher among older adults. For example, using age-based mortality rates, 37 percent of rural counties have expected mortality rates that are at least 30 percent above those for the United States among those infected compared to 10 percent of metropolitan counties. In contrast, the significantly younger population in many metropolitan areas diminishes the potential age-related risk. Nearly 42 percent of metropolitan counties have expected death rates at or below that for the United States as a whole compared to just 14 percent of nonmetropolitan counties.
Combining the influence of age and pre-existing health conditions provides an estimate of their joint impact on the risk of hospitalization or mortality among those infected by COVID-19 in a county. Though underlying health conditions are more common among older adults, the relationship is only modest in strength because other factors such as race, poverty, and occupation are also associated with underlying health conditions. For example, the incidence of pre-existing health conditions is high in the Mississippi Delta even though the population is relatively young because pre-existing health conditions are more prevalent in high-poverty areas and among Black Americans. Nonetheless, many rural counties have elevated risks because of the joint impact of pre-existing conditions and age.
As a result of age and pre-existing conditions, nearly 32 percent of nonmetropolitan counties have a combined risk more than 30 percent greater than the United States as a whole compared to just 7 percent of metropolitan counties (Figure 1). An additional 41 percent of rural counties have risks that are 15 to 30 percent above the United States overall compared to 22 percent of the urban counties. In contrast, 36 percent of metropolitan counties have a combined risk less than that of the United States as a whole compared to just 7 percent of the nonmetropolitan counties. In sum, the risks associated with COVID-19 infections are significantly higher in nonmetropolitan counties than in metropolitan counties both because the rural population is older and because pre-existing health conditions are more widespread there. In all, 74 percent of rural counties face higher risk at least 15 percent greater than the total United States because of age and pre-existing conditions, while only 29 percent of urban counties do.
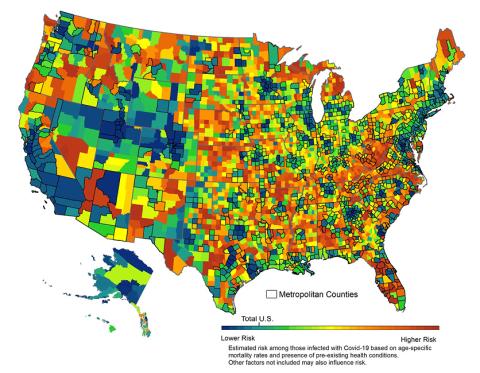
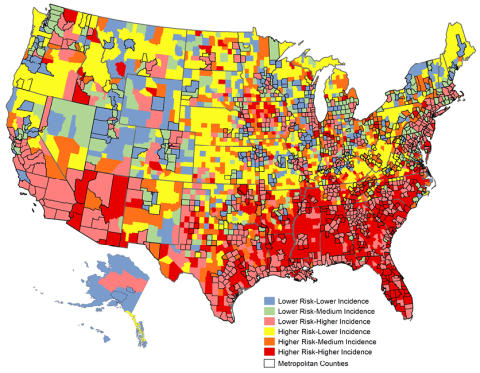
The spatial distribution of risk from the virus is reflected in Figure 2. Risks are particularly high in nonmetropolitan areas of the Appalachians and in large areas of the rural Southeast and mid-South, as well as in much of the Great Plains, northern New England, and the Upper Great Lakes, as shown in red and orange. In contrast, with the exception of Florida, the combined risks are generally lower in metropolitan areas (outlined in black) as well as in parts of the rural West, shown in blue and green.
Source: Census Bureau, CDC; A. Clark, et al. 2020, Lancet; R. Verity, et.al. 2020, Lancet. Analysis: K.M. Johnson, Carsey School, University of New Hampshire
Source: Census Bureau, CDC; A. Clark, et al. 2020, Lancet; R. Verity, et.al. 2020, Lancet; USAFacts. Analysis: K.M. Johnson, Carsey School, University of New Hampshire
Both the reported cases of the coronavirus and resulting deaths are far greater in metropolitan areas. Though metropolitan areas contain 86 percent of the U.S. population, more than 89 percent of the cases and 92 percent of the deaths from the coronavirus to date have been urban.
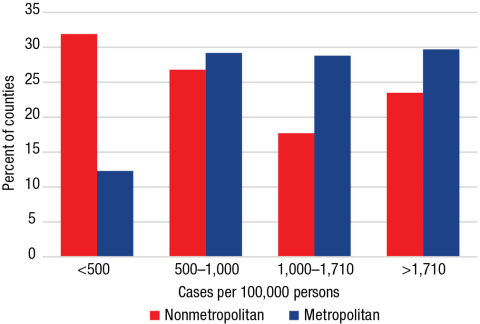
Most nonmetropolitan counties currently have had fewer cases of COVID-19 than have metropolitan counties. In the United States as a whole as of August 23, 2020, the cumulative case rate was 1,710 per 100,000 persons. But nearly 30 percent of urban counties had case rates above 1,710 per 100,000 compared to 24 percent of rural counties (Figure 3). In contrast, nearly one-third of rural counties had case rates of less than 500 per 100,000 compared to 12 percent of the metropolitan counties.
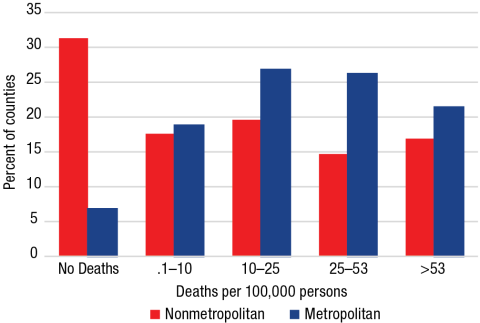
Cumulative death rates from COVID-19 also remain considerably lower in most rural counties. In fact, 31 percent of all nonmetropolitan counties had yet to experience a single COVID-19 death as of August 23 compared to just 7 percent of metropolitan counties (Figure 4). However, not all nonmetropolitan counties have been spared from high COVID-19 mortality: while the death rate for the United States as a whole is 53 deaths per 100,000 population, 17 percent of all rural counties have death rates above 53, as do 21 percent of urban counties.
Source: USAFacts 8/23/20 data. Analysis: K.M. Johnson, Carsey School, University of New Hampshire
Figure 4. COVID-19 Death Rates by Metropolitan Status
Source: USAFacts 8/23/20 data. Analysis: K.M. Johnson, Carsey School, University of New Hampshire
Nonmetropolitan case and death rates lag behind those in metropolitan areas, yet the rate of increase has become greater in rural areas. From July 1 to August 23, the number of nonmetropolitan cases increased by 161 percent and the number of deaths by 97 percent compared to 107 percent and 35 percent, respectively, in metropolitan counties. And the incidence of COVID-19 deaths is spreading. On June 1st, 59 percent of rural counties had yet to have a COVID-19 death, but as of August 23 that share had dropped to 31 percent. Among metropolitan counties the share was 19 percent in June and 7 percent in August. This is of particular concern because the older age structure and greater incidence of pre-existing health conditions put many rural counties at higher risk should infections begin to occur there (Figure 5). Nearly 32 percent of all nonmetropolitan counties are at higher risk but still have a low incidence of COVID-19 (shown in yellow).6 Many are in areas remote from metropolitan areas (outlined in black), and, should infections spread to these areas, the consequences will be serious because many have only limited access to comprehensive medical care. Many of the 25 percent of nonmetropolitan counties that are at high risk and already have high death and case rates (in red) tend to be nearer to metropolitan areas where exposure rates are higher but comprehensive medical care is also available. However, some of these counties are in areas—such as the Mississippi Delta—where poverty rates are high, a factor that limits accessibility to care even if it is proximate. As the pandemic continues and infections spread, many higher-risk nonmetropolitan counties are in jeopardy.
Source: Census Bureau, CDC; A. Clark, et al. 2020, Lancet; R. Verity, et.al. 2020, Lancet; USAFacts. Analysis: K.M. Johnson, Carsey School, University of New Hampshire
Both age and pre-existing conditions have a substantial influence on the risks from exposure to the virus, but there are other important factors. The higher levels of poverty, inequality, and food insecurity among rural populations make them more vulnerable to adverse outcomes of COVID-19. Access to health care is also a significant challenge in rural areas because there are fewer physicians, health care workers, and hospitals. Timely access to major hospitals and specialists is imperative for those with severe virus symptoms. Yet, while 14 percent of the U.S. population resides in nonmetropolitan counties, fewer than 10 percent of the ICU beds are there. Nearly 50 percent of U.S. counties have no ICU beds at all, and most of these are rural counties.7 Even the lower population density in rural America that some suggest has diminished the incidence of the virus so far is a double-edged sword. The fact that the rural population is spread across 72 percent of the land area of the country makes it easier to maintain social distance, but it also means that the specialized care only available at comprehensive medical centers is far away from many rural residents.
A substantial majority of coronavirus cases and deaths are occurring in metropolitan areas, where 86 percent of the population resides. But percentage gains in rural cases and deaths now exceed those in metropolitan counties, creating significant impacts for rural people, places, and institutions. Rural America is a deceptively simple term for a remarkably diverse collection of places8 that face unique demographic, social, and institutional challenges in dealing with the onslaught of COVID-19. The rural population is older and has more health conditions. Distances are greater, places are more isolated, and the population density is lower. These factors may have sheltered nonmetropolitan counties from the initial onslaught of COVID-19, but the situation is changing rapidly. As the virus spreads, the risk to rural populations is growing. Should the spread of the virus further disrupt the infrastructure and supply chains of rural America, it will have significant implications for the nation at large because rural America provides most of the country’s food and raw materials. The fates of rural and urban America are inextricably intertwined, so responding to the virus must address the needs of both areas.
This brief focuses on how the age structure and extent of pre-existing health conditions in counties influence the relative risks of death and hospitalization associated with the virus in rural and urban areas. Data on number of cases and deaths by county come from the USAFacts Project.9 The impact of the age structure is reflected in the estimated death rates among those infected with the virus for each county using age-specific mortality estimate from recent research on the COVID-19 epidemic in China. I applied these mortality rates to the age structure of the overall U.S. population and to that of each U.S. county using recent age estimates from the U.S. Bureau of the Census. I calculated an index comparing the death rate of each county to that for the nation as a whole.10 The pre-existing health conditions index was calculated using estimates of the proportion of the population over age 18 who have the following health conditions: obesity, diabetes, lung disease (COPD), heart disease, and kidney disease and multiple chronic conditions, using data from the Centers for Disease Control and Prevention.11 The index was constructed by multiplying the proportion of the population over age 18 with each condition by the county population over age 18 and by a weight reflecting the likelihood of hospitalization for the specific condition; summing these products and dividing by the total population over 18; then comparing this product to that for the nation as a whole.12 The mortality and pre-existing conditions indices were then added together and divided by two. The combined index compares each county to the nation as a whole. It is a relative rather than an absolute measure. It is not influenced by the proportion of a county population that is infected. So, a county with a higher estimated risk but a lower proportion of infected individuals may have less hospitalizations and deaths than a county of the same size with a lower risk but a larger proportion of its population infected.
- The terms nonmetropolitan and rural are used interchangeably, as are the terms urban and metropolitan.
- K.M. Johnson, “An Older Population Increases Estimated COVID-19 Death Rates in Rural America,” National Issue Brief 147 (Durham, NH: Carsey School of Public Policy, University of New Hampshire, 2020), https://scholars.unh.edu/cgi/viewcontent.cgi?article=1400&context=carsey; T. Marema and B.Bishop, “Rural Counties Set Record for New Cases of Covid-19,” Daily Yonder, June, 26, 2020, https://dailyyonder.com/rural-counties-set-record-for-new-cases-of-covid-19/2020/06/26/.
- R. Verity et al., “Estimates of the Severity of the Coronavirus Disease 2019: A Model-Based Analysis,” The Lancet Infectious Diseases, March 30, 2020, https://www.thelancet.com/action/showPdf?pii=S1473-3099%2820%2930243-7; A. Clark et al., “Global, Regional, and National Estimates of the Population at Increased Risk of Severe COVID-19 Due to Underlying Health Conditions in 2020: A Modeling Study,” Lancet Global Health 8:1003-17, June 15, 2020, https://doi.org/10.1016/S2214-109X(20)30264-3.
- While I recognize that factors in addition to the age structure and pre-existing health conditions will influence the risks from COVID-19 in a given area, I do not address them here. My concern is with how differences in the age structure and incidence of pre-existing conditions in rural and urban areas influence the risks from the COVID-19 virus.
- E.K Stokes, L.D Zambrano, K.N. Anderson, et al., “Coronavirus Disease 2019 Case Surveillance—United States, January 22–May 30, 2020,” Morbidity and Mortality Weekly Report 69:759–65, DOI: http://dx.doi.org/10.15585/mmwr.mm6924e2; G. Zhao et al., “Prevalence of Disability and Disability Types by Urban–Rural County Classification—U.S., 2016,” American Journal of Preventive Medicine 57, no. 6:749–56.
- For Figure 5, “higher risk” is defined as more than 15 percent above the overall U.S. and “lower risk” is 115 percent or below. Lower-incidence counties have fewer than 1,000 cases and 10 deaths per 100,000 population, medium-incidence counties have fewer than 1,000 cases or fewer than 10 deaths per 100,000, and higher-incidence counties have more than 1,000 cases and 10 deaths per 100,000 population.
- M.A. Williams, B. Gelaye, and E.M.B. Leib, “The COVID-19 Crisis Is Going to Get Much Worse When It Hits Rural Areas,” Washington Post, April 6, 2020, https://www.washingtonpost.com/opinions/2020/04/06/COVID-19-crisis-is-going-get-much-worse-when-it-hits-rural-areas/.
- K.M. Johnson, “Where Is Rural America, and What Does It Look Like?” The Conversation, February 20, 2017, https://theconversation.com/where-is-rural-america-and-what-does-it-look-like-72045.
- Data on number of cases and deaths by county come from the USAFacts Project, https://usafacts.org/visualizations/coronavirus-COVID-19-spread-map/.
- The estimated mortality rates in Verity et al. 2020 were adjusted to reflect the population age structure and the likely differential in underreporting of cases by age. Rather than use absolute death rates, which are sensitive to many conditions specific to a given country, I calculated relative death rates. Unless the basic assumption of the model that age-specific death rates rise substantially with age is incorrect, the positions of the counties relative to one another should be largely invariant.
- Data for the health conditions index from H. Razzaghi, Y. Wang, H. Lu, et al., “Estimated County-Level Prevalence of Selected Underlying Medical Conditions Associated With Increased Risk for Severe COVID-19 Illness, United States, 2018,” Morbidity and Mortality Weekly Report 69:945–50, July 24,2020, https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6929a1-H.pdf; dataset: https://stacks.cdc.gov/view/cdc/90519.
- In constructing the index, the five individual pre-existing conditions and an estimate of multiple conditions are differentially weighted to reflect varying risk of hospitalization among those infected using information from A. Clark et al. 2020.
Barbara Cook provided GIS support for this project, and Semra Aytur provided epidemiological analysis. This research was supported by the author’s Andrew Carnegie Fellowship and the New Hampshire Agricultural Experiment Station in support of Hatch Multi-State Regional Project W-4001 through joint funding of the National Institute of Food and Agriculture, U.S. Department of Agriculture. The content is solely the responsibility of the author and it does not necessarily represent the official views of the sponsoring organizations.

Kenneth M. Johnson is senior demographer at the Carsey School of Public Policy, Class of 1940 professor of sociology at the University of New Hampshire, and an Andrew Carnegie fellow.